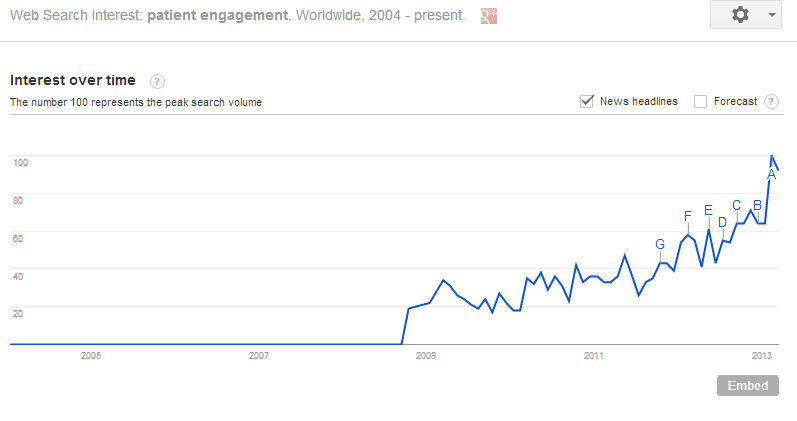
If you haven’t heard, patient engagement is all the rage- one look at Google Trends confirms that the term is being thrown around an awful lot over the last few years. Late last year, a well-known health IT consultant dubbed patient engagement the “blockbuster drug of the century.” Lofty praise, indeed.
Yes, there are not many clinicians that are anti-patient engagement. Yet, according to a 2012 study by the National eHealth Collaborative, there is a discrepancy amongst providers regarding what constitutes engagement in the vein of health IT. Without a proper definition, the phrase ‘patient engagement’ can become nothing more than rhetoric; another buzz-phrase with an abstract meaning used to influence clinicians via an appeal to their emotions. We can’t let this happen, because engaging patients throughout their course of care is truly integral in improving health outcomes.
So what is patient engagement? I won’t try to answer that question for all health care providers; I do not claim to have that much knowledge or authority. My answer is based upon a melding of current evidence with my personal experiences as a physical therapist, and should be taken as such.
Patient engagement starts and ends with patient-centered care. Patient-centered care is more concretely defined than patient engagement, and has been shown to improve outcomes, increase patient satisfaction, better enable patients, and decrease overall healthcare spending. Patient-centered care is, at its simplest, offering the patient equal say in the decision making process. It is built on:
- Establishing a personal relationship
- Maintaining an open and honest line of communication
- Being empathic
If we as clinicians offer patients a seat at the table, and simply find out what they want, we are engaging them. In most successful businesses, one of the most important metrics is consumer satisfaction. It all comes down to value: a consumer will be satisfied if he considers the services valuable.
So, what is valuable to your patients? Ask them. They’re begging to tell you. And when they do tell you, be sure that you have the ability to fulfill those needs. This is where much of health IT is missing the boat. Many clinicians are balking at the Stage 2 Meaningful Use rules that require 5% of patients to access their health records online. Their argument is they have no control over whether their patients log on or not and shouldn’t be held responsible for the lack of utilization.
If we can’t get more than 5% of our patients to actually use health IT, then we shouldn’t be calling it ‘Meaningful Use’. A clinician cannot force a patient to log on, but what they can do is provide an incentive for a patient to log on. Instead of focusing on how to meet meaningful use standards with the technology we have, we should be focusing on how to utilize technology so that it can be meaningful to our patients. We need to stop assuming we know what our patients want, and instead seek to find out.
In the end, patient engagement is a product of being a patient-centric provider. Patient engagement is contingent upon establishing a relationship built on trust & mutual understanding, maintaining open communication, and providing empathy. If we practice in this manner, we will gain a deeper understanding of the needs of each patient. Once those needs are understood, we can provide the tools necessary to meet those needs. And if we can provide online resources that solve a real problem for a patient, ‘Meaningful Use’ will no longer be a misnomer.
Ryan Klepps PT, DPT – TheraVid LLC
You can reach ryan by email ryan@theravid.com or via twitter@TeamTheraVid


